Connect With Us
Featured Articles
Items filtered by date: June 2020
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Does My Child Have an Ingrown Toenail?
 Common symptoms of ingrown toenails are redness and tenderness surrounding the edges of the nail. If your child complains of toenail pain, it may be indicative of an ingrown toenail. Additionally, there may be a discharge oozing if the nail has become infected, and it may cause severe pain and discomfort. This condition can be the result of trimming the toenails improperly, or from wearing shoes that do not have adequate room for the toes to move freely in. It may feel better when your child soaks the affected toe in warm water, as this may help to soften the skin. If you or your child has an ingrown toenail, it is suggested that you consult with a podiatrist who can offer the best treatment options.
Common symptoms of ingrown toenails are redness and tenderness surrounding the edges of the nail. If your child complains of toenail pain, it may be indicative of an ingrown toenail. Additionally, there may be a discharge oozing if the nail has become infected, and it may cause severe pain and discomfort. This condition can be the result of trimming the toenails improperly, or from wearing shoes that do not have adequate room for the toes to move freely in. It may feel better when your child soaks the affected toe in warm water, as this may help to soften the skin. If you or your child has an ingrown toenail, it is suggested that you consult with a podiatrist who can offer the best treatment options.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of Foot & Ankle Associates of Maine. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wounds That Don't Heal Need to Be Checked
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Plantar Warts Are Caused by a Virus
 Plantar warts develop on the bottom of the feet. They grow into the sole of the foot as pressure is endured from walking during the day, and can cause severe pain and discomfort. They appear as small, hardened areas, and may have black dots in the center. These develop as a result of blood vessels that grow inside the wart. Plantar warts are caused by a virus that lives and thrives in warm and moist environments. These types of places can include public swimming pools, shower room floors, and locker rooms. Patients who have a weakened immune system may be prone to getting plantar warts, in addition to people who have a history of developing this type of wart. It is suggested that you speak to a podiatrist if you have a plantar wart, who can determine what the best course of treatment is for you.
Plantar warts develop on the bottom of the feet. They grow into the sole of the foot as pressure is endured from walking during the day, and can cause severe pain and discomfort. They appear as small, hardened areas, and may have black dots in the center. These develop as a result of blood vessels that grow inside the wart. Plantar warts are caused by a virus that lives and thrives in warm and moist environments. These types of places can include public swimming pools, shower room floors, and locker rooms. Patients who have a weakened immune system may be prone to getting plantar warts, in addition to people who have a history of developing this type of wart. It is suggested that you speak to a podiatrist if you have a plantar wart, who can determine what the best course of treatment is for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Foot & Ankle Associates of Maine. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Possible Treatments for an Achilles Tendon Injury
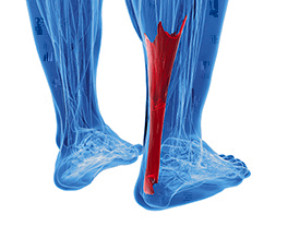 The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Foot & Ankle Associates of Maine. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
How Do You Know If You Have Developed Athlete’s Foot?
 Athlete’s foot is a contagious condition, and as its name suggests, is often common among those who participate in sporting activities. Athlete’s foot can be identified by a few different symptoms. These indicators may include cracking or peeling blisters between the toes, redness and scaling on the soles of the feet, rashes and bumps on the feet, and itchiness. Even though the name is athlete’s foot, this condition can develop for anyone. Not wearing the proper footwear in warm and moist environments can lead to developing athlete's foot, as that is where fungi tend to thrive. These environments can include public swimming pools, communal showers, gyms, and locker room floors. If you believe you have developed athlete’s foot, it is suggested that you seek the help of a podiatrist for proper and professional care.
Athlete’s foot is a contagious condition, and as its name suggests, is often common among those who participate in sporting activities. Athlete’s foot can be identified by a few different symptoms. These indicators may include cracking or peeling blisters between the toes, redness and scaling on the soles of the feet, rashes and bumps on the feet, and itchiness. Even though the name is athlete’s foot, this condition can develop for anyone. Not wearing the proper footwear in warm and moist environments can lead to developing athlete's foot, as that is where fungi tend to thrive. These environments can include public swimming pools, communal showers, gyms, and locker room floors. If you believe you have developed athlete’s foot, it is suggested that you seek the help of a podiatrist for proper and professional care.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with one of our podiatrists from Foot & Ankle Associates of Maine. Our doctors will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Every Day Foot Care
Our feet are important in our everyday lives. The problem is that we tend to neglect them. When this becomes a habit, it can cause significant trouble. Ignoring foot problems can mean pain, limited mobility, and expensive doctor's visits. On the other hand, if feet are cared for and looked after regularly, they will perform without pain or complication.
Routine hygiene is the most basic way to care for the feet. Wash and dry them thoroughly daily. Remember to get between the toes and keep the toenails trimmed and short. If the feet feel dry or there are signs of dryness or cracking, use a moisturizer designed for the feet.
When using moisturizer on the feet, try to avoid applying between the toes. If cream or lotion sits too long, they can cause fungal and bacterial growth. When moisturizer is used between the toes, it can also cause the skin to soften too much.
Shoes are also an important aspect of foot care. When one is picking out shoes, make sure they are the correct size. Shoes need to be snug, but not too tight. On the other hand, if shoes are too loose they can cause foot problems as well. It is highly recommended that shopping for new shoes be done later in the day. The reason for this is that the feet will have settled and swelled to their full size by then. To keep your feet at their most healthy, avoid wearing high heels or flip flops too often. Instead, choose shoes that are good for your feet. Good shoes pad the soles of your feet and support the arches and ankles.
Socks should also be worn daily with closed-toe shoes. They may feel hot during the summer months, but they absorb sweat and moisture off the feet. Without socks, the build-up of sweat in a closed-toe shoe can cause fungal problems and athlete's foot.
The best thing to remember in every day foot care is that shoes do make a difference. If you spend a lot of time on your feet, make sure that your shoes show no signs of wear. Shoes should offer ample support for the arches and the overall foot. Additionally, try to make foot cleaning and maintenance a daily habit. If you keep these things in mind, your feet will stay healthy and safe.